Please visit Microfungi.net for a free online course accredited by the University of Manchester, and eligible for CME/CPD points.
- Detection of fungi directly in clinical specimens – the particular appearances may be highly characteristic of certain infections, ie Zygomycete infection or India Ink in cerebrospinal fluid. Direct microscopy, if positive, is faster than culture.
- Confirmation that a culture of an airborne fungus such as Aspergillus is the cause of the infection and unlikely to be a contaminant.
- Identification of fungi, based on morphological appearances.


Staining
The oldest specific preparation for microscopy is a concentrated (10-20%) potassium hydroxide solution, which softens keratin and allows direct visualisation of fungi and some morphology evaluation. Gram stains are less sensitive. Papanicolaou stains may be useful. Cytology slides may be stained with silver stain or Grocott’s Methenamine Silver (GMS) stains. Immunofluorescence microscopy is the best method to detect Pneumocystis. Fluorescent brighteners (Calcofluor white, Blankophor or Tinopal UNPA-GX), which bind to chitin in the fungal cell wall, are a rapid means of scanning samples for fungal hyphae, and enhance morphology assessment.

CSF and meningitis
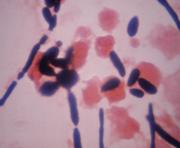
Encapsulated Cryptococcus cells can often be detected in specimens of CSF or other host fluids or secretions mounted in India ink. About 50% of HIV-negative and more than 80% of HIV-positive patients have a positive India ink examination of the CSF. However, intact lymphocytes, in particular, can be confused with the organism. In persons with AIDS, Cryptococcus cells are usually plentiful in the CSF, although the capsules can be small, making recognition difficult. Persistently positive CSF findings in patients undergoing treatment should be considered evidence of failure or relapse only if they are confirmed by a deterioration in the patient’s clinical condition or by positive cultures.
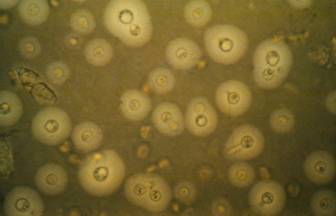
India ink preparation of CSF showing multiple yeasts with large capsules, and narrow buds to smaller daughter cells, typical of C. neoformans 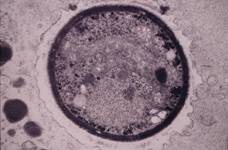
Transmission electron micrograph of a C. neoformans cell seen in CSF in an AIDS patients with remarkably little capsule present. These cells may be mistaken for lymphocytes. 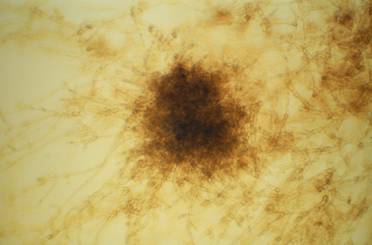
A filamentous fungus in the CSF of a patient with meningitis that grew Candida albicans in culture subsequently.

Hair
Specimens from the scalp should include hair roots, the contents of plugged follicles and skin scales. Except for favus, the distal portion of infected hair seldom contains any fungus. For this reason, cut hairs without roots are unsuitable for mycological investigation. One method that is useful for collecting material from the scalp is hair brush sampling.
Direct microscopic examination of infected material should reveal arthroconidia of the dermatophyte located outside (ectothrix) or inside (endothrix) the affected hair. The arthroconidia can be either small (2–4 um diameter) or large (up to 10 um diameter) in size. Skin scales will contain hyphae and arthroconidia. In T. schoenleinii infection (favus), loose chains of arthroconidia and air spaces are seen within the affected hairs. The scutulum (crust) consists of mycelium, neutrophils and epidermal cells.
Skin scraping showing filamentous hyphae with blankophor

Nails
The quality of the specimen taken is a major factor in success or otherwise of microscopy and culture. Having a specimen taken should be painless apart from occasional slight discomfort when subungual specimens are taken. The figure below shows the appropriate sites from which nail specimens should be obtained (Denning et al, 1995).
Scrapings taken with a blunt scalpel or clippings should be transported in a folded square of paper, preferably fastened with a paper clip, but commercial mycological packs are also available. In the laboratory 20-30% potassium hydroxide solution is added to part of the specimen to macerate the nail keratin so that the specimen can be examined for fungal elements by direct microscopy. Alternatively a part of each sample is examined in nail-dissolving solution containing a fluorochrome (Monod et al, 1989). An example of a reactive solution is this. It is prepared by dissolving 1 g Na2S in 7.5 ml distilled water and subsequently adding 2.5 ml ethanol. Thereafter, 10 ml Blankophor or 20 ml 1% aqueous solution of Tinopal UNPA-GX (Fluorescent brightener 28, F3543; Sigma) is added to this mixture.

Mucus from paranasal sinuses
A diagnostic feature of allergic fungal rhinosinusitis (AFRS) is the presence of eosinophilic mucin containing hyphae, collected from the patient’s nose or paranasal sinus cavities without evidence of tissue invasion by fungus. Hyphae may be sparse in sinus content and take considerable time to visualise with the currently used stains. Without this positive feature, other diagnoses are usually made, including allergic rhinosinusitis (ARS) or eosinophilic mucin rhinosinusitis (EMRS). However, the use of much more sensitive diagnostic techniques, such as chitin staining or specific anti-Alternaria immunofluorescence stains, may improve sensitivity. Supportive diagnostic features include the presence of Charcot-Leyden crystals, bony erosion, and heterogeneous opacity with sinus expansion on CT scan.

Otitis externa and ear canal
Debris and secretions should be obtained from the auditory canal. Direct microscopic examination will reveal branching hyphae, budding yeast cells or both. In cases of Aspergillus infection, the typical sporing heads can sometimes be seen.

Corneal scrapings for keratitis
Fungal keratitis is a medical emergency and needs to be recognized and treated promptly. For microbiological diagnosis, the best specimen is material from the affected part of the cornea; the material may be collected in the form of scrapings from an ulcerated area or biopsy when the corneal epithelium is intact and infection confined to the corneal stroma. Corneal scrapings are obtained by using an instrument such as a platinum spatula, Beaver blade, Bard Parker knife No.15 or blunt cataract knife. Cotton-tipped swabs are less effective for debriding the necrotic corneal slough. Material should be collected from the base and edges of the ulcerated part of the cornea repeatedly. If the material has been streaked onto a sterile medium, the same blade or spatula can be used again to collect additional material; however, if the material has made contact with a non-sterile microscope slide, the blade must be changed while the spatula can be flamed, cooled and then reused.
Direct microscopic examination of stained smears of corneal scrape material is the fastest means of making a presumptive diagnosis. Septate hyaline hyphae of filamentous fungi seen could represent species of Aspergillus, Fusarium or Acremonium. Coloured septate hyphae of phaeohyphomycetes such as Curvularia may be seen. Occasionally Candida spp. is the cause of keratitis and so yeasts and hyphae may be seen, suggestive of this diagnosis. Confocal microscopy may be a more direct means of establishing the diagnosis.
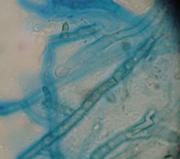
Corneal scrape with lactophenol cotton blue shows separate hyphae with Fusarium spp or Aspergillus spp.
Dr Philip Thomas, Tiruchirappalli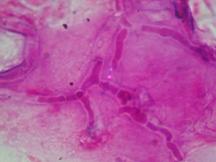
Corneal scraping stained with lactophenol cotton blue showing beaded septate hyphae not typical of either Fusarium spp or Aspergillus spp, being more consistent with a dematiceous (brown coloured) fungus
Dr Philip Thomas, Tiruchirappalli

Tissue and peritoneal fluids
The microscopic detection of typical budding yeast cells, pseudohyphae, and/or true hyphae of Candida species in tissue sections or normally sterile body fluids is indicative of invasive candidiasis. Typically, C. glabrata produces only yeast cells, and only C. albicans produces true hyphae in tissues.
Gram stain of a centrifuged fluid (in this case urine) containing C. albicans, showing the yeast and hyphal forms, so often seen in this type of specimen. 
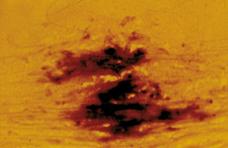
Spherules of Coccidioides immitis in an aspirate from a chronically inflamed joint from a Mexican patient in California

Respiratory samples
Sputum examination is helpful in ABPA as hyphae can often be seen with eosinophils and Charcot-Leyden crystals. Occasionally uncommon fungal infections can be diagnosed by microscopy when spherules or large yeasts such as Blastomyces dermatitidis are visualised. Aspergillus or other filamentous hyphae may be seen in bronchial wash material from fungal tracheobronchitis, sometimes with sporulating heads visible. Microscopy has a higher yield than culture in invasive pulmonary aspergillosis from BAL samples, in some centres depending on the method used. No studies have compared methodologies for microscopy or fungal culture yield.
The diagnosis of Pneumocystis pneumonia (PCP) depends on microscopy, PCR or histopathology of biopsies. Appropriate specimens for analysis include bronchoalveolar lavage (BAL) fluid, tracheal aspirate, bronchial brushing, percutaneous transthoracic needle aspiration, pleural fluid and transbronchial or open lung biopsy. Induced sputum samples are helpful only if positive; the absence of Pneumocystis from an induced sputum sample does not exclude the diagnosis of PCP.
The microscopic demonstration of typical octonucleate cysts or trophozoites of P. jirovecii in tissues or body fluids is sufficient for diagnosis. In many cases, the organisms will be present as large clusters in which it may be difficult to distinguish the different life-cycle stages. Collapsed organisms are usually found intermingled with intact organisms.
Unlike other pathogenic fungi, P. jirovecii does not bud, and this feature can be used to distinguish between this organism and others, such as small variants of Blastomyces dermatitidis, Candida glabrata, capsule-deficient Cryptococcus species and Histoplasma capsulatum. Giemsa and Wright stains detect both the cyst and trophozoite forms, but do not stain the cyst wall. Methenamine silver, periodic acid-Schiff, Calcofluor white and toluidine blue stain the cyst wall. Trophozoites and cysts can also be detected by direct or indirect immunofluorescent staining using fluorescein-conjugated monoclonal anti-P. jirovecii antibodies. Depending on the monoclonal selected, staining may target only the cyst form or all forms of the organism. Different stains perform differently, in one of the very few microscopic comparisons in mycology published (Denning et al, 1995).

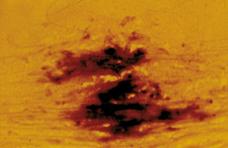
Mucous plug examined by light microscopy with KOH, showing a network of hyaline branching hyphae typical of Aspergillus, from a patient with ABPA. 
The same preparation of a BAL specimen showing hyaline, septate hyphae consistent with Aspergillus, stained with Blankophor on the left and KOH on the right. 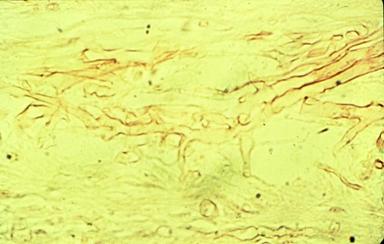
KOH preparation of a respiratory fluid showing wide non-septate hyphae, typical of a Zygomycete. 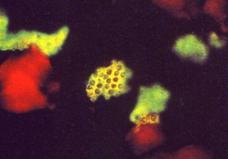
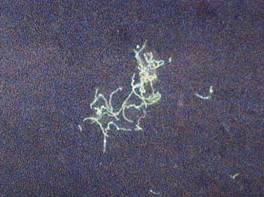
Immunofluorescence stain for Pneumocystis jirovecii in a BAL fluid (Procop et al, 2004)

Blood film or bone marrow

Mucous plug examined by light microscopy with KOH, showing a network of hyaline branching hyphae typical of Aspergillus, from a patient with ABPA. 
The same preparation of a BAL specimen showing hyaline, septate hyphae consistent with Aspergillus, stained with Blankophor on the left and KOH on the right. 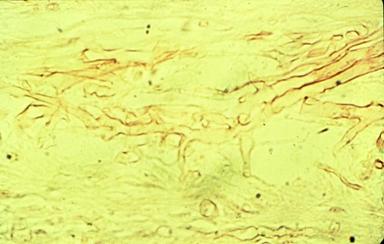
KOH preparation of a respiratory fluid showing wide non-septate hyphae, typical of a Zygomycete. 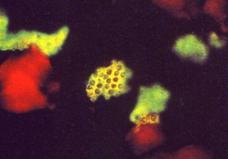
Immunofluorescence stain for Pneumocystis jirovecii in a BAL fluid (Procop et al, 2004)
The sensitivity of microscopy from blood and bone marrow is not high enough for most fungal infections to justify the time examining samples, with the exception of disseminated histoplasmosis and Penicillium marneffei, usually in AIDS. A Wright’s stain may reveal intracellular small yeasts in monocytes. These two fungi can be difficult to distinguish but P. marneffei is a fission yeast and so an intracellular wall may be seen within the yeast cell, like a belt around the waist.
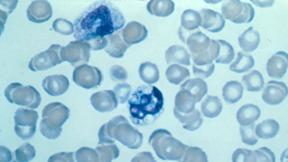
Intracellular yeasts seen in a Wright’s stained blood smear in a patient with disseminated histoplasmosis.

Candida vaginitis
The diagnosis of vaginal candidiasis depends on a combination of typical symptoms and signs and the demonstration of the fungus in smears or its isolation in culture. Culture is much more sensitive and reliable (about 90%) than microscopy (about 40%). Swabs should be taken from discharge in the vagina and from the lateral vaginal wall, and sent to the laboratory in transport medium. Microscopy of a high vaginal swab reveals yeasts with or without filaments in 40% of cases. Calcofluor white or other fluorescent brightener staining increases sensitivity.

Mycetoma grain
The diagnosis of mycetoma depends on the identification of grains which should preferably be obtained from an unruptured pustule (sinus) using a sterile needle. The roof of the lesion should be lifted off and the sinus contents, including any grains, squeezed out and placed onto a glass slide. Each grain should be picked out, rinsed in 70% alcohol, and then washed in sterile saline before being cultured. Direct microscopic examination of the grains in 20% potassium hydroxide will confirm the diagnosis of mycetoma and will also reveal whether the causal organism is a fungus or an actinomycete.
Black grains suggest a fungal infection; minute white grains often indicate a Nocardia infection and larger white grains the size of a pinhead may be of either fungal or actinomycotic origin. Small, red grains are specific to Actinomadura pelletieri, but yellowish-white grains may be actinomycotic or fungal in origin. Actinomycotic grains contain very fine filaments (<1 um diameter), whereas fungal grains contain masses of short entangled hyphae (2–4 um diameter) that are sometimes pigmented.