| Disease name and synonyms Histoplasmosis – chronic cavitary pulmonary, fibrosing mediastinal and adrenal |
| Fungi responsible Histoplasma capsulatum |
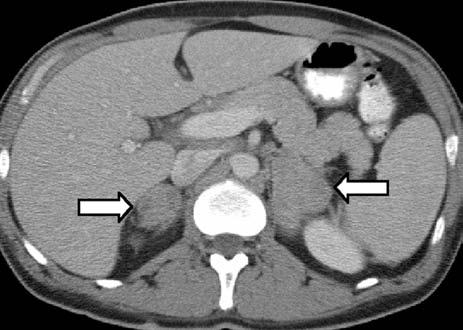
| Disease description Chronic cavitary pulmonary histoplasmosis refers to progressive cavitation of the lung in those with underlying lung disease. It is usually bilateral and involves the upper lobes. The presentation is similar to chronic pulmonary aspergillosis with productive cough, increasing shortness of breath, weight loss, night sweats and sometimes fever. Fibrosing mediastinitis follows acute pulmonary histoplasmosis in a small number of patients. While mediastinal lymphadenopathy is often a prominent feature of acute histoplasmosis, fibrosing mediastinitis is not directly related to this. Patients present with recurrent pneumonia, haemoptysis or respiratory failure. Superior vena cava obstruction, narrowing of pulmonary arteries or veins and narrowing of the major airways is common on detailed assessment. It is progressive. Occasionally adrenal histoplasmosis occurs. These patients present with chronic fatigue, but usually adrenal function is preserved, although addisonian symptoms (difficulty swallowing, extreme weakness, fainting, low blood pressure) may be precipitated by initiation of anti-tuberculous therapy (rifampicin induction of cortisol metabolism). Adrenal nodules are found on CT scans. Biopsy reveals the organism. |
| Frequency and global burden All unusual or rare complications of histoplasmosis. |
| Underlying problems and at risk patients Chronic pulmonary disease, especially COPD is usual for chronic cavitary pulmonary histoplasmosis. No specific underlying diagnosis has been identified for fibrosing mediastinitis or adrenal histoplasmosis. |
| Diagnostic testing Sputum or bronchoscopy culture is usually positive for H. capsulatum in chronic cavitary pulmonary histoplasmosis. The laboratory should be warned of the possibility of Histoplasma as it is a class 3 pathogen. In fibrosing mediastinitis and adrenal histoplasmosis, radiology provides the most obvious clue to the diagnosis. Histoplasma antibody is usually detectable but biopsy, if possible, provides definitive evidence of disease. |
| Treatments Itraconazole 200-400mg daily, assuming no drug interaction with rifampicin. Therapeutic drug monitoring is recommended. IDSA Clinical Practice Guidelines 2007 |
| Outlook and prognosis Adrenal histoplasmosis can be cured with antifungal therapy. Adrenal function maybe suboptimal and needs checking. Fibrosing mediastinitis is progressive and incurable currently with a mortality of >30%. Chronic cavitary pulmonary histoplasmosis can be arrested with antifungal therapy, with residual pulmonary damage being the major on-going problems. |