Subcutaneous mycoses occur when fungi become implanted under the skin. This is often seen in agricultural labourers. While dissemination is rare, mycoses can cause significant disfigurement and disability, especially if not treated promptly. Fungi can also be implanted under the cornea, usually as a result of trauma. For more information please see our section on fungal eye infections.
Mycoses occur more often in people living in underdeveloped, rural areas in tropical and sub-tropical regions. The most common implantation mycoses are described below, but there are many more (e.g. lacaziosis/lobomycosis, phaeohyphomycosis, zygomycosis). For a review of implantation mycoses in Latin America please see Queiroz-Telles et al (2011). You can also access the GAFFI factsheet on mycetoma.

Clinical lectures & awareness videos

Mycetoma
For more information about mycetoma please visit the website of the Mycetoma Research Centre in Khartoum, or follow them on Twitter @MycetomaRC or YouTube. Mycetoma is classified as a Neglected Tropical Disease by WHO.
You can also access the Life Worldwide factsheet on mycetoma.

Chromoblastomycosis
| OVERVIEW For reviews see Queiroz-Telles et al (2017), or read the detailed GAFFI factsheet Chromoblastomycosis (CBM) is a cutaneous and subcutaneous mycosis characterized by the appearance of proliferating chronic skin lesions following traumatic implantation of the fungus. Sites most commonly affected are the lower limbs. Upper limbs and buttocks are also frequently involved. Outbreaks on ear, face, neck and breasts have been occasionally reported. Lesions start out as a nodule or papule, that slowly enlarge becoming verrucose and wart-like. Old lesions can be tumorous or cauliflower-like in appearance. Lymphatic and hematogeneous dissemination have been described, but they are infrequent. |
| FUNGI Many melanised (black fungi) fungal species can be the etiologic agents of this disease. The most frequent are: Fonsecaea pedrosoi complex (includes F. monophora and the species formerly known as F. compacta) and Cladophialophora carrionii. Less common species involved are Phialophora verrucosa, Rhinocladiella aquaspersa, Exophiala spp and new Fonsecaea species. |
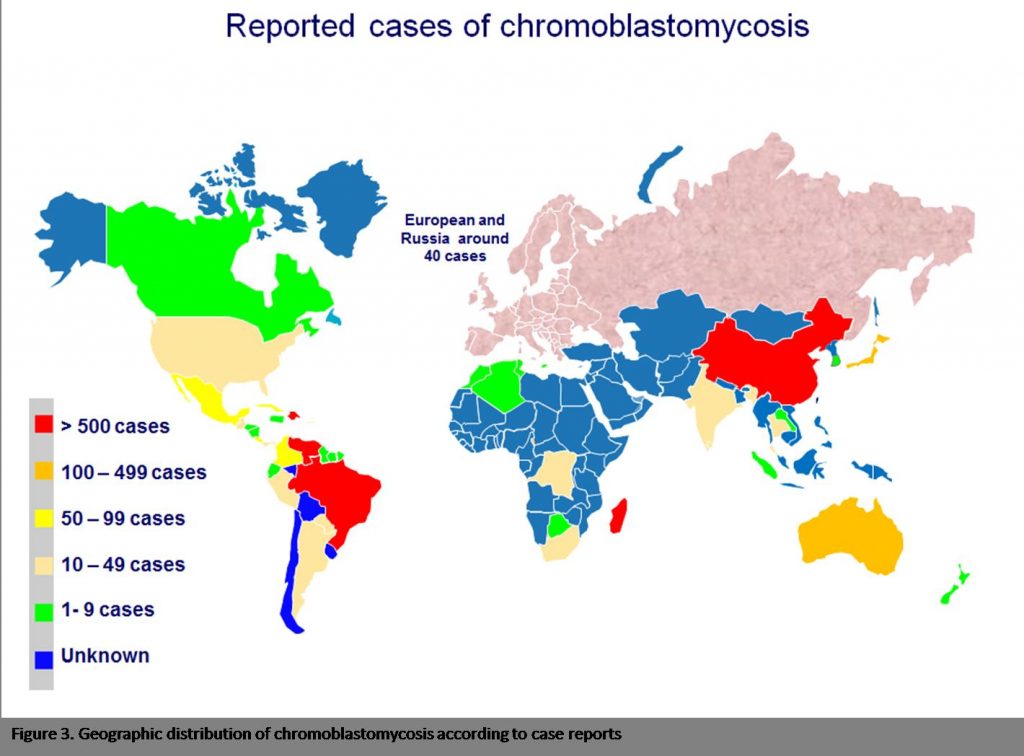
| GLOBAL BURDEN This condition occurs worldwide, but the frequency is much higher in tropical and subtropical areas of Africa, Central and South America, Asia and Australia. Global burden is unknown. In high endemic areas the incidence can reach 16 cases per 100,000 inhabitants. |
| RISK FACTORS This disease is occupational and relates to activities that can cause traumatic injury and contact with contaminated material. It is frequently observed in agricultural labourers. |
|
DIAGNOSIS To establish a diagnosis of chromoblastomycosis, rounded sclerotic bodies, planate dividing and brown pigmented, should be observed in the clinical samples. To identify the etiologic agent, clinical samples should be cultured on isolation media, such as Sabouraud agar. Great expertise is needed to identify these fungi to species level. It is advisable to perform the identification by means of Internal Prescribed Spacer (ITS) sequencing. |
| TREATMENT Topical imiquinod (an TLR7 agonist) has proven to be effective for small lesions (de Sousa, 2014). |
| OUTLOOK Small and localized lesions have a good prognosis. Cure is difficult when the lesions are large. Most common complications are ulceration and secondary infections and lymphoedema. |

High power image of a typical image of highly characteristic ‘muriform’ cells seen histologically during infection. Muriform bodies have a brown (melanin) surface layer and are seen within a chronic inflammatory infiltrate with granulomas and micro abscesses 
Typical micromorphology of F. pedrosoi complex 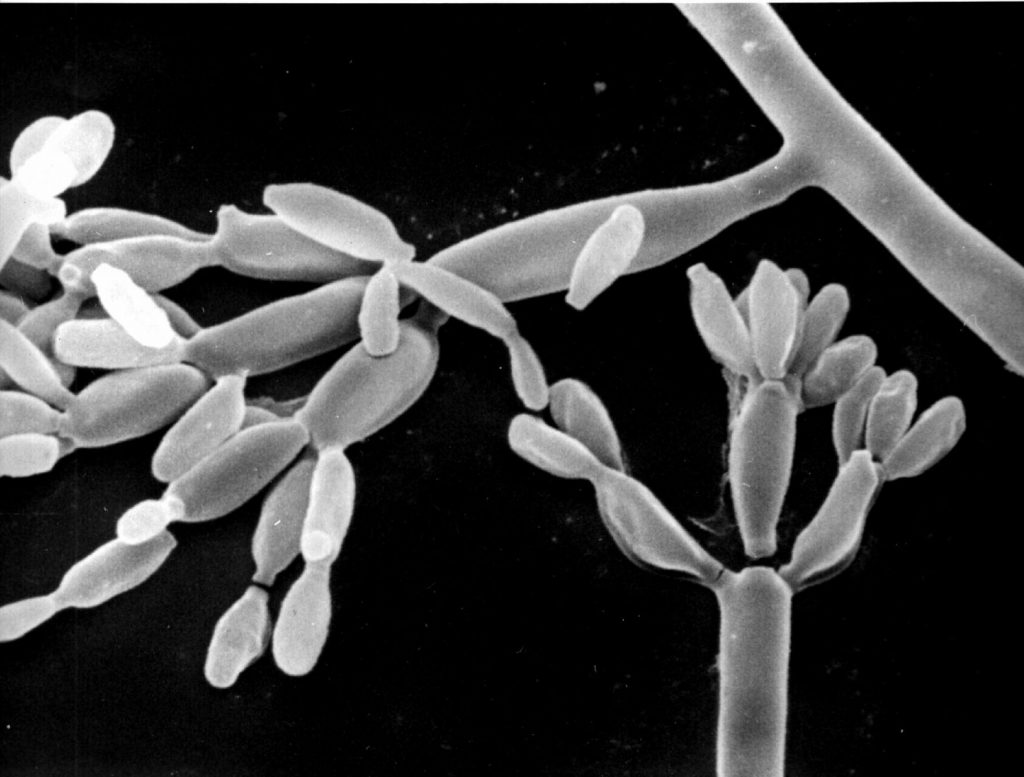
SEM image of F. pedrosoi complex

Facial chromoblastomycosis from Papua New Guinea 
Severe facial and ear chromoblastomycosis in a man from Papua New Guinea 
Chromoblastomycosis of the arm in a woman from Papua New Guinea. 
Chromoblastomycosis of the arm in a woman from Papua New Guinea. 


Sporotrichosis
| OVERVIEW Sporotrichosis can occur when fungus is implanted under the skin following minor trauma, such as handling thorny plants or a bite/scratch from an infected cat. Immunocompromised patients, and those with diabetes or alcoholism, are at increased risk of sporotrichosis developing into a life-threatening disseminated disease. The vast majority of cases of sporotrichosis have lymphocutaneous disease or localised ulceration of the skin, without nodules or lymph node swelling. Disseminated disease occasionally occurs with multiple skin nodules, osteoarticular disease, especially affecting large joints, and meningitis. Pulmonary sporotrichosis is also reported by rare, presenting similarly to subacute invasive pulmonary aspergillosis. |
| FUNGI Sporothrix schenckii complex (includes S. albicans, S. brasiliensis, S. globoa, S. luriei, S. mexicana and S. schenckii). [ teleomorph = Ophiostoma stenoceras ] Isolated from soil, wood and plant matter Read more at Dr Fungus |
| GLOBAL BURDEN Sporotrichosis has been reported worldwide, with most cases coming from Central and South America (Mexico, Colombia, Brazil, Peru) and parts of China. Hyperendemic rural areas may have attack rates of 1 case per 1000 of the population. In northern India, ~30% of inhabitants in villages where sporotrichosis had been reported had evidence of exposure to the organism compared with 6% in villages without clinical cases. Point source outbreaks have been know to occur. These have been traced to infected cats, certain mosses and hay. Please see the review by Chakrabarti et al (2014). |
| RISK FACTORS Farmers, gardeners and forestry workers are at increased risk of sporotrichosis. Those affected are usually healthy adults, under the age of 30, but young children can also be infected. S. schenckii most commonly enters the body through traumatic implantation, but only a minority of patients recall any history of trauma. AIDS may also lead to disseminated sporotrichosis. |
| DIAGNOSIS The best test to identify sporotrichosis is a skin biopsy with both histopathological examination and fungal culture. Aspiration can lead to false negative results, as organisms are scanty. Antibodies directed against S. schenckii may be detected in blood in those with disease, but are particularly valuable to diagnose meningitis. This is due to S. schenckii, as cerebrospinal fluid (CSF) cultures are invariably negative, but yield specific antibodies. Skin testing with Sporothrix antigen is usually positive in patients with this disease and may be a useful diagnostic tool (Bonifaz, 2018). |
| TREATMENT A saturated solution of potassium iodide and itraconazole is the treatment of choice. Side-effects of potassium iodide include metallic taste in mouth, salivary gland enlargement and rash. Terbinafine 250 mg twice daily is also highly effective. Fluconazole is less effective, as all isolates are resistant. Amphotericin B is initially useful for disseminated and meningeal disease, although micafungin may be more active, followed by itraconazole. Sporothrixio spp are resistant to voriconazole. In pregnancy, local heat (42-43ºC) application to the lesions, over several months, may be effective. |
| OUTLOOK Excellent for cutaneous and lymphocutaneous disease, with cure rates exceeding 95%. Meningeal and pulmonary sporotrichosis are difficult to diagnose and treat, with less positive outcomes. |

Multiple lesions on the arm typical of the lymphocutaneous form of sporotrichosis 
Appearance of a nodule in the skin lesion which is an early feature of sporotrichosis 
An ulcerated case of sporotrichosis in a gardener 
Ulcerated lesion caused by S. schenkii

Lobomycosis (lacaziosis)
A rare infection characterised by keloid-like nodules on the ears and limbs, particularly among men working outdoors in the Amazon basin. Caused by Lacazia loboi. Also affects dolphins. See Francesconi et al (2014) or Araújo et al (2018).